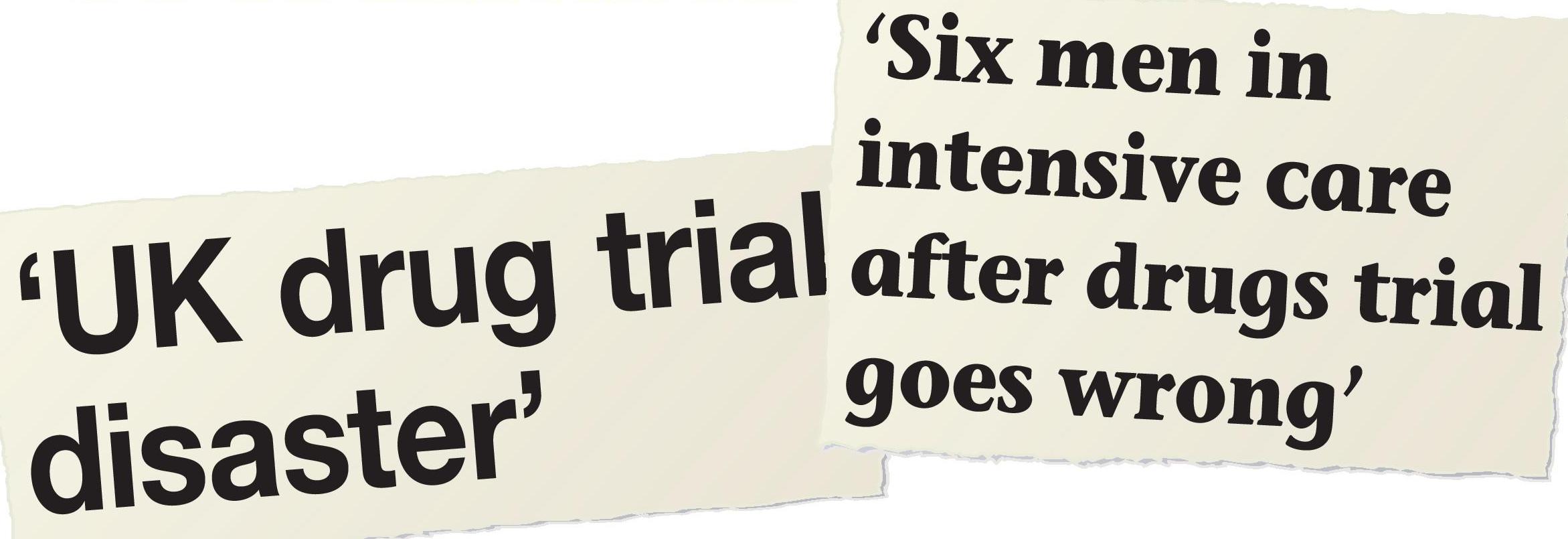
In 2006, six seriously ill volunteers were admitted to intensive care after taking an experimental drug (a monoclonal antibody — see pp. 30–34, this issue) as part of a clinical trial at Northwick Park Hospital. The volunteers all had multiple organ failure. This incident made headline news and sparked serious concerns among the public about drug testing, even though all six volunteers survived. Testing new drugs in humans is a type of clinical research called clinical trials of investigational medicinal products (IMP), so-called because the investigation is conducted in a clinical setting, such as a hospital. People often think that clinical trials (of IMP) consist of volunteers who are paid to take an experimental drug but there are many types of clinical trials. Clinical research is one of the most heavily regulated industries in the world.
Many years of detailed research on a new drug are necessary before testing in humans can begin. This research involves both in vitro studies (such as tests on blood samples) and in vivo studies (research on living organisms). In vivo studies may include animal testing. Some people think that research involving animals is unethical but the tests are necessary to gain an idea of the drug effects in humans. Many drugs fail to reach the stage of drug testing in humans. They may be too toxic, or not show enough benefit. If a drug is shown to be safe enough, research will then be conducted in human subjects (in a clinical trial). This is necessary as the drug’s effects may be quite different in humans than in other animals. This is clearly demonstrated by the Northwick Park disaster — the monoclonal antibody that had such disastrous consequences for the human subjects had an excellent safety profile when previously tested in non-human primates.
Your organisation does not have access to this article.
Sign up today to give your students the edge they need to achieve their best grades with subject expertise
Subscribe




